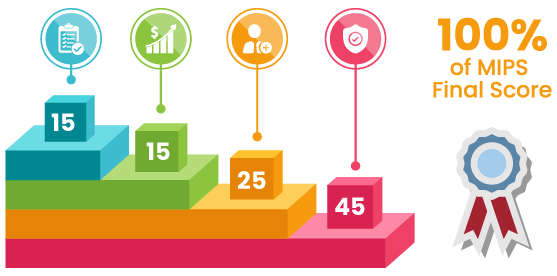
- Improvement Activities – 3 months
- Promoting Interoperability – 3 months
- Cost – 12 months
- Quality – 12 months
If you use P3 consulting for submissions before April 30, 2020, you can expect a positive payment adjustment in 2021.
The Quality Payment Program (QPP) under Medicare Access and CHIP Reauthorization Act (MACRA) enters into the third year in 2019. CMS 2019 Final Rule brings a few changes to the Merit-Based Incentive Payment System as it works to accommodate the eligible professionals (EPs) and hospitals. In the end, whether it is the government authorities or CMS itself, they are on a mission to empower the patients and their health in an ideal healthcare system.
P3, as a MIPS consulting service, commits to these changes and arranges them for participants of MIPS 2019.
If you use P3 consulting for submissions before April 30, 2020, you can expect a positive payment adjustment in 2021.











Here, we narrate the low volume threshold or the minimum requirements for participating in MIPS 2019.
There are three characteristics to qualify in this program, which is one more than in 2018.
If you are below the above criteria, you do not qualify for the MIPS program in 2019.
Furthermore, if you are taking part in an Advanced APM and enrolled for the first time in Medicare in 2018, consider your status in the current year as ‘Not Eligible’.


Quality Payment Program Participation Status Tool available at the QPP website puts you in a position to know your real-time eligibility status.
As a MIPS consulting service, we can check it on your behalf. All we need is your National Provider Identifier (NPI).
Let’s do this!
P3 offers three extraordinary packages to support these data submissions keeping the prerequisites of quality reporting intact.
The above options can get you home without negative payment adjustments on your 2021 Medicare reimbursement. The adjustment rises to 7% in 2019 from 5% in 2018.
Go here to read the list of MIPS Quality measures. Give us a call or visit the QPP portal to learn more. 1-844-557-3227 is your go-to number.
MIPS Qualified Registries submit most of the Quality measures. However, the submissions happen according to the measures (high-priority, outcome) supported by submission types. Generally, EHR, eCQMs, Qualified Registry, and Claims are the four types of submission methods. When you submit the same measure through more than one submission type, only the best score will go in your final figure.
We don’t take more than 30 minutes of your time to shortlist measures.
Shortlist measures with mutual agreement and report to CMS confidently
We require a few minutes to train the practice manager/staff on the coordination process. As we are in this business for years now, the intelligence is already there to finalize and begin activity implementation
According to the CMS 2019 Final Rule, more clinician types enter into the program and if they are unable to score a minimum of 30 points, they are subject to -7% payment adjustments. 7% of your Medicare reimbursement is a big amount and not easy to digest.
P3 Healthcare Solutions will continue to post updates on MIPS so that there is no room for confusion. It is an honor for us to report MIPS on behalf of individual clinicians as well as groups (virtual groups included) for the past 2 years. Schedule a meeting today to discuss your financial and reputation career with us.
For questions out of this service, or on instructions on how to get started call a HIT consultant today at 1-844-55-P3CARE or email at info@p3care.com.
What do you think is the right mode of MIPS data submissions?

