While providers are serving in healthcare with a passion for putting patients first, CMS has always well-performed its part to make healthcare safer and affordable for all. Merit-based incentive payment system with its deeper entanglement with MACRA is one of the steps taken by the US government under its Quality Payment Program. For providers who invest in patients’ health by facilitating their patients with a quick response and considerable care, the Merit-based Incentive Payment System has paved a route for getting reimbursements in the form of MIPS payment (either penalties or incentives). So, after completing 6 years of its valued contributions to the provider’s professional reputation and financial aspects, we are now ready to report for MIPS 2023. That’s why P3Care has opened its doors for all providers to cater MIPS consulting and MIPS reporting services throughout the performance year 2023.
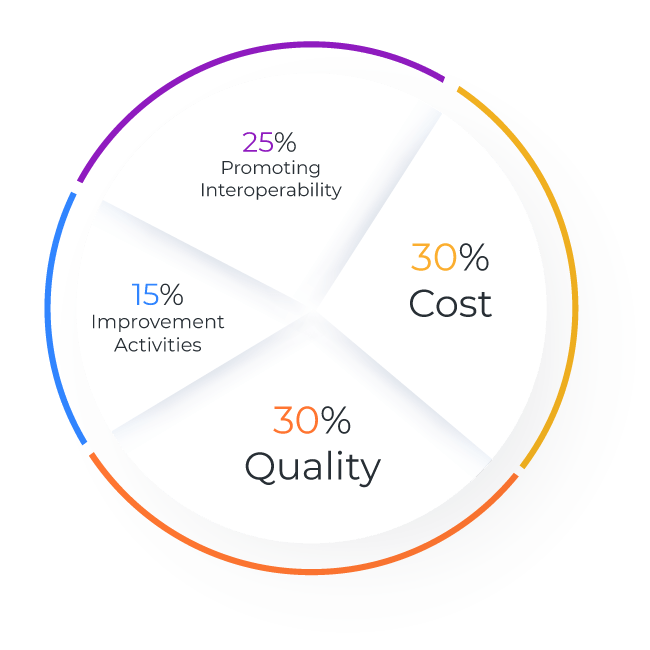
The quality payment program is moving with its strategic objectives. Thereby, it has come up with some policy updates. This year, the Centre for Medicare and Medicaid Services is destined to promote meaningful provider participation through its MIPS reporting program along with improved healthcare. Thereby, QPP challenges the limits of healthcare with its MIPS reporting program. It invites all eligible clinicians to report a relatively more connected and cohesive set of measures. This will allow CMS to provide comparative feedback with their payment adjustments