Struggling with evolving MIPS guidelines and time-consuming reporting? Our consultants provide end-to-end support to help you optimize performance scores, minimize reporting errors, and maintain full compliance

Our years of experience reflect our reliable and data-driven incentive payment solutions that benefit the revenue cycle.
P3Care’s consultancy includes a seamless approach right from data collection to MIPS quality measures submission.
We analyze every measure via a proactive approach to ensure the accuracy of your data before it reaches the CMS door.
From the eligibility check to MIPS quality measures selection to the data submission, we are with you at every step.
Improve accuracy, boost efficiency, and stay on track with your incentive goals—backed by knowledgeable support that fits your practice.
Participating in MIPS can help you avoid payment penalties and maximize incentive opportunities, and we’re here to support you throughout the process.
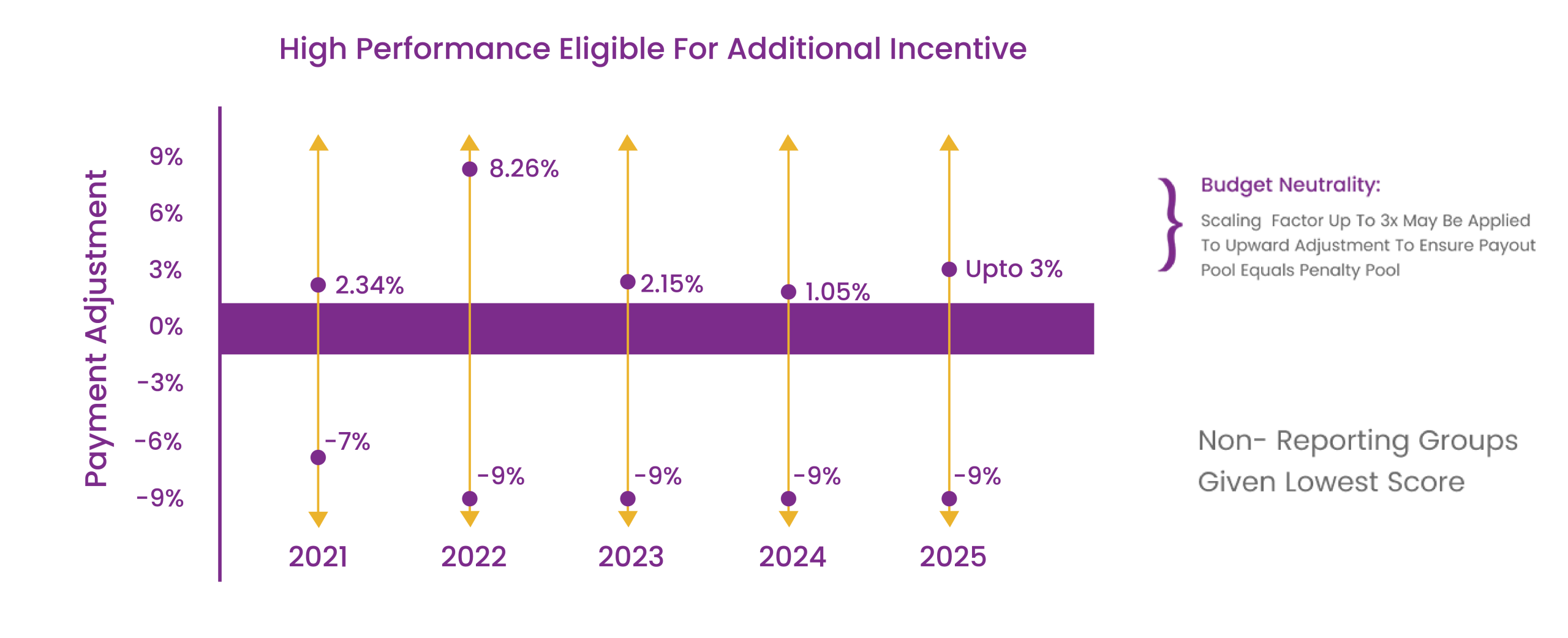
Clinicians who are eligible but do not participate may face negative payment adjustments.
Eligible clinicians have the opportunity to earn positive payment adjustments by successfully participating in the program.
CMS updates incentive and penalty rates regularly to encourage clinician participation and improve quality care outcomes.