

Getting medical bills right really depends on things being accurate, consistent, and having good, clear talks between doctors, hospitals, and insurance companies. CPT codes are just how medical billing talks to everyone else; they’re the standard language. At P3Care, we know that CPT coding is a really big deal for getting paid right and keeping our billing compliant. Even little mistakes in coding can mess with how much money we get back.
This blog aims to be a full, easy-to-read guide, breaking down CPT coding from the very start all the way to its real-world use.
A CPT code is a five-digit numeric code which healthcare providers use to identify medical procedures and professional services they deliver to patients. The American Medical Association (AMA) maintains Current Procedural Terminology (CPT) codes which are used to describe medical procedures and professional services.
CPT codes use standardized language to express medical services which insurance companies can process according to their requirements.
For example:
The purpose of a CPT code is to represent a specific service-diagnostic, surgical, anesthetic, or medical-to ensure that anywhere the same service is performed, it will be billed as a consistent procedure code.
CPT coding is not just about assigning numbers—it directly affects a healthcare organization’s financial health and compliance.
CPT coding helps to:
Without CPT codes, insurers would have no consistent way to identify what services were provided, making reimbursement unreliable.
CPT stands for Current Procedural Terminology.
This standardized terminology allows healthcare providers, payers, and auditors to speak the same language when it comes to medical services.
A standard CPT code consists of:
Modifiers explain how or why a service was different from the usual procedure. They are critical for avoiding incorrect bundling of services.
Common modifiers include:
A patient visits a clinic for a consultation and also receives a minor procedure during the same visit.
Modifiers clarify that both services were separate and should be reimbursed individually.
CPT codes are used throughout the healthcare billing lifecycle, including:
CPT codes are typically submitted with ICD-10 diagnosis codes, which explain the medical reason for the service.
It’s important to know the differences between CPT codes and other coding systems in order for you to correctly bill. P3Care monitors this distinction to help avoid errors and also help avoid rejected claims through your typical billing processes.
| Code System | What It Represents | Why It Matters |
| CPT | Procedures and services | Determines reimbursement |
| ICD-10 | Diagnosis or condition | Justifies medical necessity |
| HCPCS | Supplies and equipment | Covers non-physician services |
Simple explanation:
The process for CPT coding is a detailed, repetitive series of steps that consists of several components:
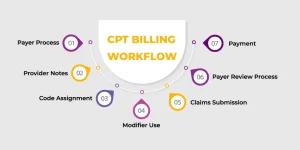
Payer Process
A patient has an encounter with a provider and receives treatment.
Provider Notes
The provider documents each service provided in the patient’s record.
Code Assignment
The coder analyzes the documentation and assigns the appropriate CPT code(s).
Modifier Use
Modifiers are assigned to provide more specific information about the service(s) provided if needed.
Claims Submission
CPT and ICD-10 codes are submitted to the payer.
Payer Review Process
The payer reviews the submitted claim(s) for accuracy and compliance.
Payment
Once the payer has completed the review process, payment will be made according to their CPT and payer guidelines.
CPT codes are divided into three main categories.
| Category | Purpose | Example |
| I | Common services | 99213 |
| II | Quality tracking | 4010F |
| III | New procedures | 0555T |
Here are commonly used CPT codes and how they are applied:
Example Scenario:
A new patient comes to the clinic and receives a consultation and lab tests. The CPT codes 99203 and 80050 would be used together for this purpose.
CPT coding errors can lead to serious financial and compliance issues.
Common mistakes include:
Even a single coding mistake can result in denied claims or delayed payments.
To ensure clean claims and consistent reimbursement:
Accurate CPT coding also supports:
Improper coding can raise red flags during payer audits and lead to penalties.
CPT coding continues to evolve with healthcare innovation:
These changes aim to improve accuracy, efficiency, and transparency in medical billing.
In medical billing, CPT codes are considered to be the foundation for proper healthcare reimbursement. These codes help ensure that medical services are properly documented, billed, and reimbursed. If applied correctly, CPT coding reduces errors, promotes compliance, and enhances the revenue cycle process as a whole. P3Care considers CPT coding as a strategic process for achieving financial stability and quality patient care.
A CPT code is a numeric identifier consisting of five digits used to describe services delivered by healthcare professionals.
The insurance company is made aware of the services delivered, how they were delivered, and how they will be reimbursed based on the rules set regarding medical necessity.
Yes, they are standardized across the country; however, the reimbursement may vary based on the provider’s contract, location, and insurance company.
The wrong use of a CPT code may result in denied claims, which is why accurate use is important in medical billing.
The modifiers provide further details regarding services delivered, allowing insurance companies to make accurate determinations regarding services that were delivered so that they are not denied.

