Every aspect of healthcare billing needs to be accurate because even minor errors have the potential to create payment delays, claim denials and compliance problems. An entity code functions as one of those essential elements which need proper identification. The technical term requires a basic understanding because its knowledge helps medical practices achieve time and financial savings and headache reduction.
The guide serves your needs if you have ever wondered why your claim was rejected or who needs to be included in your claim information. The expiration of your investigation will provide you with knowledge about entity codes and their importance and the ways medical billing and coding services prevent claim denials while enhancing claims processing. Companies like P3Care rely on these codes to ensure claims are submitted correctly and get paid faster.
The identification code which medical claims use to show healthcare transaction participants and their respective functions is known as the entity code. The claim includes this code to identify each participant in the claim process. The system guarantees that the payer of the claim receives complete identification of the healthcare provider who delivered treatment and the billing organization and the patient who received treatment.
The lab test claim requires three entity codes which include one for the physician who ordered the test and one for the laboratory that conducted the test and one for the patient who required the test. Payers need these codes to identify whom to reimburse and which services were delivered because their absence causes reimbursement and service identification issues that result in payment delays and service denials.
Entity codes exist as essential components within electronic claim systems which use ANSI X12 837 claims that have become standard across the United States healthcare industry. The codes establish a common language for all claims which enables insurance companies and clearinghouses to handle the claims processing work without any difficulties.
Entity codes aren’t just random letters and numbers — each code represents a specific role on a claim. Understanding these roles is essential for accurate claim submission.
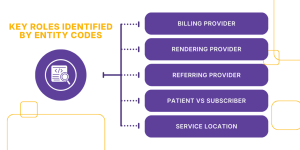
The billing provider is the person or organization that submits the claim. This could be a clinic, hospital, or physician’s office. The billing provider code to identify the organization that handles payment processing and claim submission to the payer system uses code 85 in claims.
Example: Dr. Smith performs a procedure at his clinic. The clinic submits the claim because it operates as the billing provider despite Dr. Smith providing the service.
The rendering provider is the clinician who actually performed the service, such as a physician, nurse practitioner, or lab technician. Entity codes for rendering providers (like code 82) allow the insurance company to know who performed the treatment or procedure.
Example: The nurse who performs lab work for Dr. Smith shows yet another example of a rendering provider.
The rendering provider is the clinician who actually performed the service, such as a physician, nurse practitioner, or lab technician. Entity codes for rendering providers (like code 82) allow the insurance company to know who performed the treatment or procedure.
Example: The nurse who performs lab work for Dr. Smith shows yet another example of a rendering provider.
Some entity codes distinguish between the patient receiving the service and the subscriber — the person whose insurance policy covers the claim. This distinction is critical for claims where a dependent receives care under a parent’s insurance.
Example: A child sees a pediatrician. The child is the patient; the parent is the subscriber.
Certain entity codes designate where care was provided — for example, hospital, outpatient clinic, or telehealth visit. This helps payers understand the setting of service for proper adjudication and reimbursement.
Understanding these roles is essential for anyone involved in medical billing services, ensuring that each claim accurately reflects the care provided.
Entity codes may seem like minor details, but their impact is huge. Accurate codes are critical for:
Correct entity codes enable payers to process claims because they provide accurate information about claims which need to be interpreted. The process of submitting a claim results in faster payment times which helps medical practices maintain their financial operations.
The absence of valid codes or their incorrect use and their absence from claims leads to claim denials. Denial of claims requires staff members to dedicate their time to claim correction and the resubmission process which results in revenue delays.
P3Care and other medical billing service companies use entity codes during their claim scrubbing process to identify errors that need correction before they submit claims. The medical facility achieves better revenue cycle management because accurate entity coding enables efficient handling of patient registration through to payment collection.
The ANSI X12 electronic claim standard includes entity codes which comply with HIPAA regulations. The universal claim format enables payers to read and process claims correctly which decreases compliance risk..
This section is about typical errors in entity coding and why they matter. The mistakes listed are common but can have serious consequences:
Overall Impact:
Takeaway: Paying attention to entity codes prevents errors, saves time, and ensures faster reimbursement.
Understanding entity codes requires knowing several related terms in medical billing. Here’s a detailed explanation:
Takeaway: Knowing these terms is crucial to understanding how entity codes fit into medical billing operations and why they matter for medical billing and coding services.
This section covers practical steps to avoid errors and optimize the revenue cycle:
The tiny technical elements of entity codes actually function as essential components which create correct healthcare billing processes. The codes provide identification of which person performed each task on the claim, which results in quicker payments and reduced claim rejections and improved legal adherence.
Entity codes function as essential knowledge for medical billing optimization when you operate your billing department either through internal staff or specialized services from P3Care. A small detail, when done correctly, can make a huge difference in your practice’s financial health.
An entity code serves as a distinct identifier which enables healthcare claims to demonstrate the functions of each involved person such as the billing provider, rendering provider, or patient. The system guarantees precise claim evaluation which results in quicker payment processing.
Entity codes prevent three main issues which include claim denials and claim delays and compliance problems. They enable payers to identify service providers and billing parties and insured individuals which simplifies the process of managing revenue cycles.
Common errors include swapped provider roles, missing patient/subscriber codes, outdated NPIs or TINs, and not updating codes when payer requirements change. The mistakes result in claim denials which cause payment delays and require extra administrative tasks.
You can verify entity codes by:
Yes. P3Care Medical Billing Services provides professional billing services that ensure precise claim preparation through proper entity code implementation. The process of outsourcing decreases errors which results in better claim approval and improved cash flow management.

