Did you know that accurate pathology billing can directly impact a lab’s financial stability, with Medicare payments set to decrease by 2.4% in 2025?
Pathology medical billing is essential for labs to ensure they are properly reimbursed for their services. As of 2025, the global medical billing outsourcing market is projected to reach $39.98 billion, driven by the growing complexity of billing processes and the demand for specialized expertise.
In 2025, the medical payment for the pathology lab will face a 2.4 % decrease, continuing a trend of reduced reimbursement rates since 2021. Additionally, the 2025 CPT codebook has introduced over 270 new codes, including 101 related to genetic testing and digital pathology, further complicating billing practices.
Pathology medical billing is the process of submitting claims to insurance companies for laboratory services such as diagnostic tests and tissue samples. Laboratories provide CPT (Current Procedural Terminology) codes to describe the services rendered by them. Proper coding is crucial to the billing process to ensure labs get reimbursed correctly.
At the core of medical pathology billing, it is important that the billing is done appropriately to have a steady cash flow and to avoid claim denials.
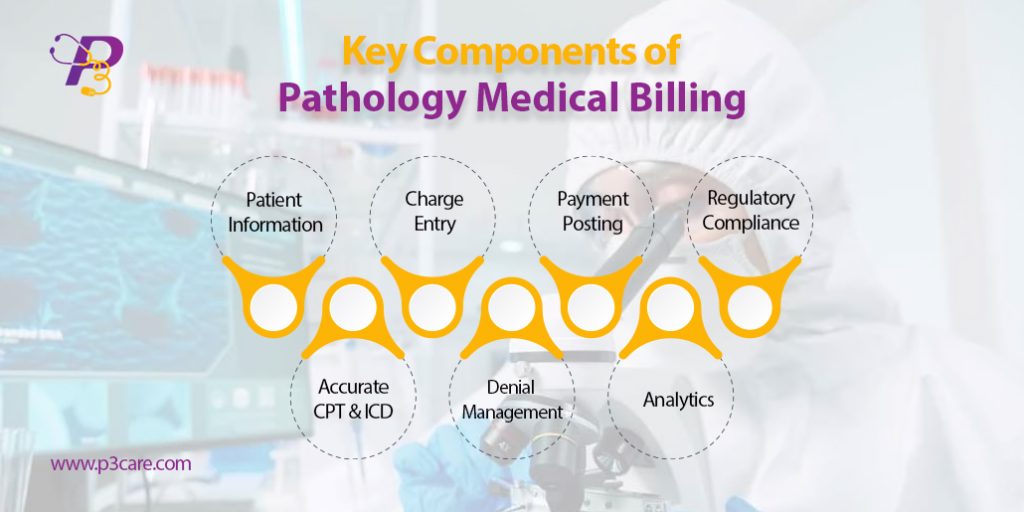
To ensure maximum reimbursement and error-free claims, it’s crucial to understand the building blocks of pathology medical billing. These components are essential for labs and billing teams to streamline the revenue cycle and reduce claim denials.
Accurate demographic entry and insurance verification are foundational. Even minor errors in patient data can lead to rejections or underpayments.
According to MGMA, nearly 24% of denied claims result from eligibility-related mistakes.
Each pathology test must be properly documented with the ordering provider’s signature, ICD-10 diagnosis codes, and proof of medical necessity.
Applying up-to-date pathology CPT coding guidelines is critical. Coders must understand distinctions between technical and professional components and use modifiers such as -26 and -TC correctly.
Clean claims—those free of errors—are submitted electronically. This accelerates approval and minimizes delays.
Having a system in place to track, appeal, and correct denied claims ensures labs don’t lose revenue due to avoidable issues.
Every Explanation of Benefits (EOB) must be matched with charges, ensuring payments are posted correctly and underpayments are flagged.
Regulations from HIPAA, CMS, CLIA, and PAMA must be followed rigorously. Labs should conduct periodic audits to stay compliant.
Monitoring KPIs like clean claim rate, Days in A/R, and denial trends helps improve long-term performance.
Billing services for pathology labs go far beyond basic claim filing. These services are designed to handle high-volume lab operations while ensuring accuracy, compliance, and faster cash flow.
Labs that use professional billing services see a 20–30% increase in claim approval rates.
By partnering with a provider that specializes in billing services for pathology labs, labs gain a competitive edge and peace of mind.
Following the correct pathology CPT coding guidelines is non-negotiable. Every test billed must match the correct CPT and ICD-10 code, especially when working with government and commercial payers.
Stay up to date with annual changes. The 2025 CPT code updates will impact certain molecular pathology and lab panel services.
Accurate coding not only protects your revenue but also shields your lab from audits and compliance violations.
Many pathology groups and labs are now turning to outsourced pathology billing companies to reduce costs, improve collections, and stay compliant in a complex billing landscape.
Reporting and trend analysis
P3care is trusted outsourced pathology billing company, which means focus on your core operations or lab testing and patient care, while the experts handle your billing.
The world of pathology medical billing is evolving rapidly. New technologies, stricter compliance standards, and changing payer behavior are all reshaping how pathology labs manage their revenue cycles.
Fact: Labs using AI in their billing process reported a 25–30% reduction in claim denials (HFMA 2024).
Every year, CPT coding changes have a direct impact on billing operations. The 2025 CPT code updates for pathology introduce new codes, retire outdated ones, and adjust descriptors to better reflect current lab practices.
AI is no longer the future—it’s now actively transforming clinical pathology billing solutions across the industry.
Automates payment posting and EOB reconciliation.
Insight: AI adoption in pathology billing is projected to grow 40% per year through 2027
Here are some current statistics that highlight the state of pathology billing in 2024–2025:
Average Days in A/R for high-performing labs: 25 days (vs. industry avg. 42 days).
Pathology medical billing is more than a back-office function—it’s a core revenue driver. With constant changes in CPT codes, payer policies, and compliance regulations, pathology labs need to stay informed and proactive. P3Care manages billing in-house or works with an outsourced pathology billing company. Investing in technology, training, and expert support is the key to long-term financial health.
A: It involves managing both clinical and anatomical codes, applying correct modifiers, adhering to ever-changing payer rules, and justifying medical necessity. These layers of complexity make billing accuracy and compliance a constant challenge for labs.
Q2: What are the top reasons pathology claims get denied?
A: Common reasons include incorrect CPT codes, mismatched diagnosis codes, missing modifiers, and insufficient documentation. Regular coding audits and continuous staff training are essential to reducing denials.
A: At least once a year, especially after the AMA releases CPT code updates. However, quarterly reviews are recommended to keep up with payer-specific changes and evolving compliance guidelines.
A: Yes, outsourcing can significantly reduce administrative burden, improve cash flow, and ensure compliance. A trusted partner like P3Care helps streamline the process with certified coders and real-time reporting tools.
A: Outsourcing to experienced billing professionals enhances claim accuracy, reduces denial rates, and speeds up reimbursements. It also allows labs to focus on testing and diagnostics while companies like P3Care handle the financial side.

