The healthcare industry requires efficient insurance claim management as its main operational focus during modern times. CPID in Medical Billing—short for Claim Patient Identifier—functions as a distinct identification number that healthcare facilities use to track and manage their claims process. Clinics face the danger of claim mistakes and delayed payments because they lack CPID and they must deal with excessive work.
A patient who visits a medical facility multiple times during one month creates a situation where his claims might become confused without a CPID, which leads to delays in revenue collection and distress for patients. P3Care provides a smooth and automated workflow to streamline operations and enhance claim processing efficiency.
In this article, we’ll cover everything about CPID—from its definition, workflow, software applications, challenges, best practices, and even future trends—so you can fully understand its importance in modern medical billing.
A Claim Payer Identifier (CPID) serves as a distinct identification number that insurance companies use to track each insurance claim. The CPID functions as a claim-specific identification system that enables users to monitor payment processes and claim denials and track claim progress.
The CPID plays a key role in ensuring each claim is processed correctly. Benefits include:
Example: John Smith visits a clinic three times in one month. Each visit generates a separate CPID, allowing the billing team to manage claims individually, avoiding mix-ups and delayed payments.
CPID vs Other Identifiers
It’s important to distinguish CPID from other identifiers used in medical billing.
| Identifier | Purpose | Example |
| Patient ID | Identifies the patient in the hospital system | PID12345 |
| CPID | Identifies a specific insurance claim | CLM56789 |
| Payer Claim Number | Assigned by insurance | PCN98765 |
| Account Number | Reference to the billing account | ACCT1122 |
Key takeaway: CPID is claim-specific, not patient-specific. A patient may have one Patient ID but multiple CPIDs. Software managing multiple CPIDs seamlessly, reducing errors and administrative work.
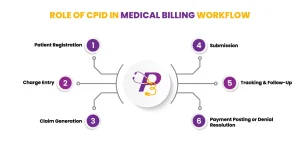
CPID helps ensure accurate communication with clearinghouses:
Using CPID, billing teams can resolve denied claims efficiently.
Common denial reasons:
Example: A claim rejected for coding errors can be corrected and resubmitted using the same CPID, ensuring accurate tracking and faster payment.
CPID is implemented in most billing systems, including:
Example: Each claim automatically generates a CPID linked to the patient and visit, minimizing manual tracking errors. Screenshots of CPID fields in these systems help new staff understand the process quickly.
Proper CPID usage supports HIPAA compliance by:
Tip: Regular audits verify that CPIDs match patient records and claims, reducing compliance risks.
Even experienced teams face challenges:
Solutions:
Example: A clinic using CPID-focused workflows reduced claim errors by 40% and decreased payment delays by 25%
Case Study: A mid-sized hospital struggled with 500+ claims per month. Claims were often delayed or denied due to misidentification. After implementing CPID tracking:
Story: John had three visits in one month. Before P3Care, claims got mixed up, delaying payments. With P3Care’s unique claim tracking, all claims were processed correctly—ensuring smooth, accurate reimbursements.
Why Choose P3Care?
Take the next step: Streamline your claims and maximize reimbursements with P3Care today!
The CPID system functions as a crucial component of medical billing for successful claim processing and denial management and revenue collection activities. The combination of CPID knowledge, best practices, and P3Care expert practices to achieve better claim processing results while decreasing mistakes and receiving payments on schedule.
The healthcare industry now requires proper CPID management because it serves as a fundamental element of contemporary medical billing systems.
The Claim Patient Identifier CPID functions as a distinct identification number that insurance companies use to track their claims. The system enables billing personnel to maintain separate control of each claim, thus preventing any items from being misplaced or combined with other claims.
A Patient ID identifies a patient in the hospital or clinic system, while a CPID identifies a specific claim for that patient. The system enables separate tracking of multiple claims that belong to the same patient.
Yes, each visit, procedure, or insurance claim generates a separate CPID. The billing process benefits from this system because it enables teams to handle each claim as an individual case which helps them to avoid making mistakes and experiencing confusion.
CPID allows billing teams to locate and correct denied claims quickly. By referencing the CPID, they can resubmit claims accurately, track follow-ups, and ensure timely payments.
Most EHR or billing systems display the CPID in claim details. This lets staff quickly identify and track claims without manually cross-checking patient information.
By uniquely identifying each claim, CPID prevents misfiling, duplicate claims, and payment delays. It ensures that each claim follows a clear workflow from submission to payment.
The CPID system helps providers to achieve three goals, which include organizing their billing operations and decreasing their administrative tasks, and stopping revenue losses that result from mistakes. The system proves most beneficial to clinics that process large quantities of claims.
Yes, CPID provides a clear record for each claim, which helps to create better auditing processes. Auditors can track individual claims without confusion, ensuring compliance with regulations.

