The essential role of authorization in medical billing processes remains unrecognized by many people. The majority of healthcare practitioners discover the value of authorization only after their claims face rejection and their payments experience delays and their patients obtain surprise invoices.
Insurers use authorization to grant medical service approvals which medical providers need before delivering treatment to patients. The process of proper authorization protects organizational revenue while maintaining legal requirements and enhancing patient contentment. This guide provides all necessary information about authorization which professional medical billing services and medical billing and coding services use to assist practices with their authorization needs.
Authorization, also called prior authorization, pre-authorization, or pre-certification, is a process where an insurance payer reviews and approves a healthcare service before it’s performed.
It ensures:
Even if a patient has active insurance, services may be denied without proper authorization. This is why medical billing services are crucial to managing this process accurately.
Authorization impacts both revenue and patient care through its two main effects. The main reason for claim denials occurs when authorization is not obtained.
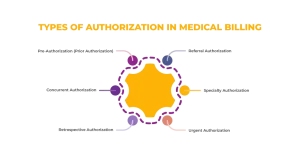
There is a requirement for prior authorization before some services, like surgery, MRI, or specialty drugs. Missing authorization will usually result in denial.
It is necessary for treatments that are continuous like long hospital stays or rehabilitation that require periodic review from the insurance company.
A service is typically requested after, and especially in, emergencies, carrying the disadvantage of being rejected more frequently.
Referral authorization exists for situations where a primary care provider needs to obtain specialist approval to treat a patient.
Some insurance plans require both a referral and authorization before specialist visits or procedures.
Specialty authorization applies to high-cost or specialized services which include cardiology procedures and oncology treatments and pain management injections and advanced imaging services.
The services require specific documentation which establishes the need for medical treatment.
The emergency procedures that need urgent approval because they are time-critical need special permission which doctors must obtain.
The insurers will expedite their requests but they still need to present necessary documentation before they can receive approval.
| Type | Definition | Example | Process Flow Summary |
| Pre-Authorization (Prior Authorization) | Approval required before non-emergency services or procedures. | MRI scans, surgeries, specialty medications | Request → Insurer review → Approval or denial |
| Concurrent Authorization | Approval required during ongoing treatment to confirm continued medical necessity. | Extended hospital stays, rehabilitation therapy | Ongoing updates → Insurer review → Continued approval or adjustment |
| Retrospective Authorization | Approval requested after services are provided, usually in emergencies. | Emergency surgery, urgent hospital admission | Service delivered → Request → Insurer review → Approval or denial |
| Referral Authorization | Approval required to visit a specialist after a primary care provider referral. | Cardiologist visit, specialist diagnostics | PCP referral → Insurer review → Patient schedules specialist |
| Specialty Authorization | Approval for high-cost or complex specialist procedures or treatments. | Oncology treatments, advanced cardiology procedures | Specialist request → Insurer review → Approval or denial |
| Urgent Authorization | Approval for time-sensitive or emergency care where delays can harm the patient. | Trauma surgery, emergency interventions | Immediate care → Post-service request → Insurer review → Approval or denial |
Medical billing and coding services ensure these steps are completed correctly to prevent denials.
The authorization process needs multiple steps which require different parties to work together between providers and billing teams and insurance companies. Exact execution of each step is necessary because approval processes will be delayed and claims will be denied if even one detail is missing.
Why this matters: Practices that rely on medical billing services and medical billing and coding services achieve higher approval rates, faster claim processing, and fewer administrative headaches.
The administrative burden arises from dealing with different payer regulations.
The reasons for denials arise from three specific factors which include documentation errors and incorrect coding and service exclusion.
Medical billing and coding services maximize approval success by:
This improves approval rates and streamlines the billing workflow.
Efficient authorization management minimizes errors, reduces delays, and optimizes revenue:
Result: Higher authorization approvals, faster reimbursements, and reduced stress for staff and patients.
Certain specialties require more prior approvals:
Focusing on these specialties allows medical billing services to reduce denials, while medical billing and coding services ensure accurate coding for complex procedures.
Authorization processes are evolving with technology and industry changes. Here’s what providers should know:
Many insurers are adopting ePA systems, allowing faster submission, real-time tracking, and reduced paperwork.
Some insurance companies are streamlining prior authorization rules to reduce administrative burden for providers.
Artificial intelligence is increasingly being used to review documentation, detect coding errors, and predict denials before submission.
Efforts are underway to standardize authorization processes across payers, making it easier for providers and billing teams to comply.
Authorization is a cornerstone of medical billing. Properly managed, it:
Professional medical billing services and medical billing and coding services bring expertise, accuracy, and compliance. They ensure:
By integrating these services into daily operations, healthcare providers can streamline workflows, reduce administrative burden, and maintain a healthy revenue cycle.
No. Authorization depends on the type of service, payer rules, and patient insurance plan. There are certain procedures which need prior approval before they can be performed.
It varies. Some approvals get processed instantly while other approvals require multiple days to complete because of payer requirements and service complexity.
No. Authorization confirms coverage but does not replace proper claim submission or correct coding. Denials can still occur if documentation or codes are incorrect.
Typically, either the healthcare provider or their medical billing services partner. Providers frequently assign billing teams to handle this process because it improves their operational efficiency.
Yes. Most authorizations have time limits. After an authorization period ends, any service that gets performed requires resubmission to prevent service denial.

