Running an OB/GYN practice is no easy job, especially when you have to deal with the tricky world of medical billing. Even small mistakes in billing or coding can end up costing your practice a lot of money. Gynecology billing is especially complicated because there are so many different procedures, constant updates to CPT codes, and insurance rules that change from one provider to another. All these challenges can lead to claims denials, delayed payments, and extra paperwork, which can put a strain on your practice’s finances and make it harder to focus on patient care.
In this blog, we will walk you through the essentials of OB/GYN billing services in 2025. You will learn about the common CPT codes, how to submit claims correctly, and what new trends you need to watch for. Whether you are just starting out or want to make your billing process smoother, this guide will give you practical tips to avoid errors and get paid after and keep the practice running strong.
OB/GYN billing services focus specifically on the medical billing needs of obstetrics and gynecology practices. Unlike general medical billing, gynecology billing involves unique challenges like managing global bundles, specialized procedure codes, and the correct use of modifiers.
For example, maternity care often requires billing for a package of services over several months, which differs from the typical single-visit billing seen in other specializations.
In 2025, studies show that up to 40% of OB/GYN claims face denials or rejection due to coding errors or incorrect modifier usage. According to a recent survey, nearly 30% of OB/GYN practices reported revenue loss directly linked to billing inefficiencies. specialized billing service is even more critical.
Dedicated OB/GYN billing ensures claims are coded accurately and submitted properly, helping to stay compliant with the insurance regulations and avoid costly delays. By reducing these error practices, practices can protect their revenue streams and minimize the administrative load, allowing providers to focus on delivering quality care to their patients
Accurate coding is one of the critical components of submitting clean claims in obstetrical and gynecological billing. Here, P3Care will present a comprehensive analysis of the CPT code categories commonly used in OB/GYN, along with live scenario examples to assist you in avoiding errors in 2025 and denials.
A routine patient visit is an Evaluation and Management (E/M) visit coded by CPT codes, 99202, 99215, which are new and established patient visits, and each is coded based on the complexity (decision-making) and time (Overall) spent with the patient and the type of visit. The E/M coding for preventive service visits, such as wellness-check visits, is done by the following CPT codes: 99381 – 99397.
The physical exam is often age-based, and health screenings are included in several of the visits. Among the often bundled preventive services is the Pap smear, which is authorized as part of a pelvic/clinical breast exam (CPT G0101), which is billed to Medicare.
Live Scenario: A patient presents for her annual exam, which includes her pelvic and breast exam. In this case, the visit coding includes 99396 for the preventive visit; when it is billed to
Medicare, G0101 is the code embedded.
Missing the appropriate incapacity modifier (such as -25 Modifier) or coding this visit as a problem visit instead of a preventive visit can provide a denial or underpayment.
Typically, diagnostic procedures done in the GYN practice consist of ultrasounds and colposcopies, with some codes being:
76801 – Ultrasound, pregnant uterus, first trimester
76830 – Transvaginal pelvic ultrasound
57454 – Colposcopy of the cervix, biopsy, and endocervical curettage
58100 – Endometrial biopsy
An issue commonly seen in 2025 is that many payers are restricting rules on who can bill diagnostic procedures. They are now insisting that we also code the diagnosis codes (ICD-10), along with justifying the linkage of the procedure to the diagnosis code.
As an example, a payer may deny a claim for a billing of the transvaginal pelvic ultrasound (76830), if the indication for the procedure is something like pelvic pain (R10.2), unless it is clearly documented in the clinical note that the procedure was medically necessary – putting the clinician at risk of a defensible audit or denying a claim.
Tip: Always document any medical necessity for a procedure, especially repeated procedures, such as colposcopy.
Many OB/GYN practices do many of the surgeries they perform in office or in their outpatient facility, these types of surgeries have higher reimbursement values but also have increased documentation risk.
58300 – IUD insertion
58120 – Dilation and curettage (D&C)
58140 – Myomectomy (removal of fibroid)
58150-58294 – Range of hysterectomy procedures depending upon type and approach
What to watch for: Starting in 2025, the misuse of modifiers (such as –51 for multiple procedures or -59 for distinct procedural services) remains one of the most common reasons for denials in surgical billing. Whenever possible, match the procedure code to the notes in the surgical report to avoid having it done again under the value of a surgery!
Maternity care is billed with global OB codes. These global codes incorporate antepartum visits, labor and delivery, and postpartum care in one bundled payment.
The most utilized codes are:
59400 – Routine vaginal delivery including prenatal and postpartum care
59510 – Routine cesarean delivery including global care
59610 – Vaginal delivery after previous c-section (VBAC), including global care
Why is this important: These codes assume the care is provided over 9-10 months, until the end of the postpartum period, and billing incorrectly incurs a large loss of revenue.
Example – If your patient transfers care mid-pregnancy, you must then use split billing codes (rather than the global code).
Pro insight: Many players in 2025 now require itemized submission of visits outside of the global period (i.e., complications, additional ultrasounds). If you do not itemize or separate those visits, you may inadvertently underbill.
Knowing and applying these CPT codes correctly is not only important to getting paid, but it is equally important to be compliant, thereby reducing denials and keeping your practice running efficiently. This is important whether you bill in-house or utilize outsourced billing.
Obstetrics and gynecology claims often have delays or denials due to incorrect modifier use. Modifiers add clarification to services, as they may not be fully described by the code alone. OB/GYN billing has scopes of services that usually involve both evaluation and procedure services, so modifiers are an important factor to consider in protecting thousands of dollars in revenue each month.
Use to demonstrate that an evaluation occurred with a procedure in the same visit, and both were medically necessary.
A patient presents with pain during a routine check-up. You provide a full E/M service, plus you conduct a separate pelvis ultrasound. You would add modifier -25 to the E/M code.
Insurance carriers are notorious for denying claims of -25 that do not have proper documentation to support separate visitation, and all insurance providers flag -25 for audit purposes. If you have a billing partner like P3Care, one of the ways we help limit the risk of audit denials is by providing a process to review and proper justification before claims are submitted.
Use to indicate that two “[separate] procedures” were performed at different times for a patient on the same date of service that normally would be bundled together.
Overutilization or misuse of -59 may produce unwanted audits in 2025. A good partner that provides a billing service like P3Care will also help you with audits of coding and training to help ensure you don’t over-utilize and stay compliant with the contract you completed with the payer.
Indicates that more than one procedure was performed during a visit. Some payers will auto-apply, but you still need to report properly on the claim.
You can let your billing software, or even a billing service like P3Care, handle -51 placement. This can help avoid double-dipping, or unintentional underpayment.
Used when the procedure is substantially more complex and time-consuming than is typical. Be ready to supply detailed operational reports. Many practices miss out on added reimbursement here due to poor documentation.
-76 is for a repeated procedure by the same provider; -77 is if a different provider does it. You always want to indicate why the procedure was repeated—change in condition, non-conclusive results, etc.
Even the best modifier won’t save a claim if the documentation doesn’t support it. In general, the payer’s rules have gotten tighter in 2025, especially in gynecology billing and coding. Here’s how to ensure that your documentation is clean and your claims are solid:
You should always make it clear in your documentation why you performed every procedure, especially when you are using a modifier like –25 or –59.
This is a must when using codes that contain an E/M visit or modifier –22.
Properly link ICD-10 to CPT: For example, link R10.2 (pelvic pain) to a diagnostic ultrasound CPT.
There are companies like P3Care that provide compliance checks with feedback loops to provide continuous improvement around documentation standards that change with payer expectations.
According to P3Care reports, nearly 28% of claims were modified –25 submitted are denied up front due to lack of documentation or insufficient support — 70% of denied claims can be reversed by making the association with documentation correct and supported.
Even if your coding is perfect, that is merely half the battle. In OB/GYN billing services, the real victories happen when your claim workflows are smooth, precise, and responsive to your needs, from when the patient walks into the office until the day reimbursement hits your bank account.
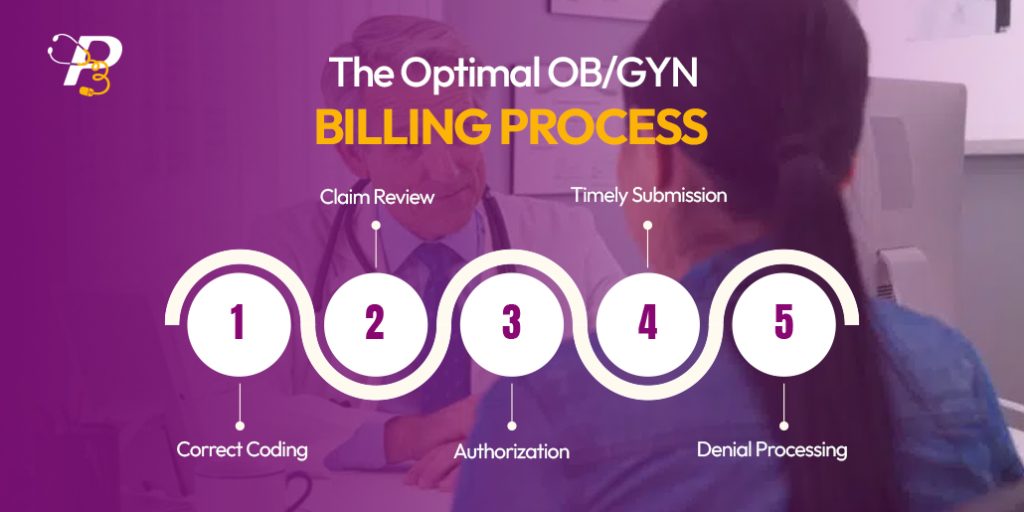
In 2025, the leading OB/GYN practices are following optimized billing workflows combining automation, real-time checks to ensure accuracy, and using data smartly to combat denials. Here’s how to create one that works — and where most practices fail.
It begins with accurate CPT and ICD-10 coding. Every service — whether it’s a Pap smear or hysteroscopy — must be coded accurately and detailed in the clinical notes.
Claims review tools identify issues, including incorrect diagnosis coding, incorrect modifiers, or incorrect structure. This might sound simple, but as P3Care’s 2025 report outlines, just claim checks prevent as much as 30% of denials!
Checking a patient’s insurance before their visit verifies coverage and prior authorization for services provided. Forget to check, and even with clean claims, timely payment may not happen.
Claims should be submitted within 24-48 hours of the patient’s visit. Late submission runs the risk of payer-specific filing deadlines, particularly for Medicaid or HMOs.
Denials and underpayment issues need to be marked, corrected, and resubmitted as soon as possible. Practices utilizing denial processing tools (like those provided by P3Care) see reso
Modern OB/GYN practices are utilizing smarter tools to expedite claims success:
Analytics dashboards (with dashboards, you can watch KPIs, including denial rates, AR days, reimbursement timelines)
According to 2025 data from P3Care, practices using full-cycle billing automation have up to a 35% error reduction and are getting reimbursed 2x faster than manually processing claims.
ICD-10 Alignment: Always use accurate, updated ICD-10 diagnosis codes that correspond with CPT codes. Billers need to be aware of codes that do not match up – in OB/GYN, that would include codes such as R10.2 (pelvic pain) and Z01.419 (routine GYN exam), which are both subject to instant rejection.
Payer-Specific Bundling Rules: Not all payers use the same bundling rules for a service. If a payer bundles an ultrasound claim with an E/M code, they will only pay for that if it is clearly documented as a separate service. P3Care track payer-specific patterns and can isolate coding issues before they are submitted, which is incredibly valuable.
In 2025,appeal, especially if the resubmission is document-heavy.
It’s vital to have a process that allows fast appeals, and your documentation needs to be attached to the SOAP notes, operative reports, and modifiers to give more chances for approval.
In 2025, the most common causes of OB/GYN claim denials include:
Common CPT codes for preventive visits include 99381–99397 (age-specific wellness visits). If a separate service like a Pap smear or diagnostic exam is provided during the same visit, a modifier –25 should be added to the E/M code to indicate a significant, separately identifiable service. For Medicare, Pap smears are often billed using G0101.
Global OB codes (e.g., 59400, 59510, 59610) should not be used if:
These modifiers are critical for reimbursement:
Caution: Both are frequently audited. Without detailed documentation, claims with these modifiers may be denied or flagged for review.
To reduce denials and optimize reimbursement:
Modern OB/GYN practices are leveraging:
Practices using full-cycle billing automation see up to 35% fewer errors and get paid twice as fast compared to manual systems.
P3Care specializes in OB/GYN billing with:

